Smart Healthcare Hub

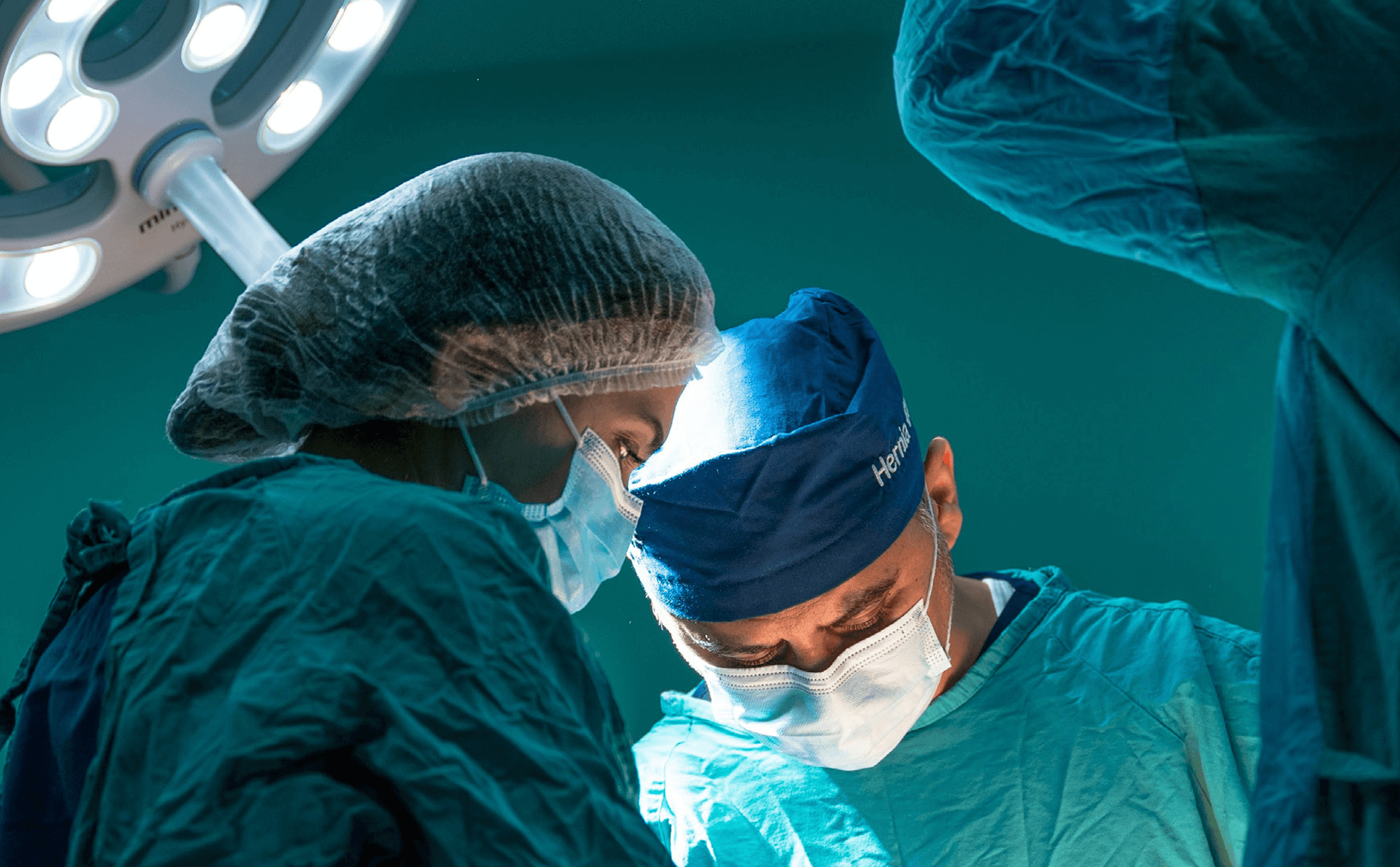
About Our Work
We conduct innovative research on implementing healthcare technologies to create safer and more effective care for patients and better experiences for caregivers, using a human-centered approach. Building on the differentiating work across engineering, liberal arts, medicine, and computer science, this interdisciplinary team seeks to fill the gap between discovery and sustained implementation of interventions to improve patient health.
Technology is a tool that can enhance and extend human capabilities, but it cannot substitute for the human interaction. Our team seeks to think beyond the next great technological discovery to the implications for frontline users and the impact to clinical work. No matter how impressive the technology might be, if it does not fit into the workflow of clinicians or does not appeal to patients, it will not be used. Our research targets holistic evaluation to ensure that AI and other technology solutions drive healthcare value without simply contributing to the ever expanding “model graveyard” of unused tools.
Contact us: smarthealthcarehub@vt.edu
On the Frontlines
Healthcare in the U.S. faces urgent challenges: Rising costs, clinician burnout, and poor outcomes have underscored the need for more efficient, patient-focused systems.
Culture of Collaboration
As a land grant university, VT is committed to serving the community and Commonwealth of Virginia. Blacksburg is located exactly 4 hours from both the richest and poorest counties in the United States. Our team has a unique partnership with a rural-serving healthcare system, Carilion Clinic, which allows us unique insight into integration of technology across different patient and clinician user groups.
In addition to its strengths in medicine and leadership in biomedical innovation, Virginia Tech has long-standing recognition in many areas directly applicable to the work of the Smart Healthcare Hub. We believe that ingenuity arises when we work in multiple dimensions and from multiple points of view. The Hub is engaging with multiple VT colleges, including the colleges of Engineering, Science, Liberal Arts and Human Sciences, and Architecture, Arts, and Design.
The Virginia Tech Institute for Creativity, Arts, and Technology (ICAT) is home to a collaborative research environment called the Cube, a reconfigurable immersive environment that hosts research ranging from embodied data analytics to cutting-edge creative work. ICAT’s methods and capabilities translate well into other kinds of immersive environments, allowing the Smart Healthcare Hub to benefit from state-of-the-art simulations enhanced by projections and audio environments.
Future collaborators may come from the Virginia Tech Transportation Institute, which has extensive experience building multisensory testbed environments. It also has a deep history of human-centered design to optimize the human user experience, and significant leadership in biomedical innovation.
Our Roadmap

Current Research Topics
- AI as a tool for human-centered healthcare delivery, (Nick Rider)
- healthcare data privacy and cybersecurity (Denis Gracanin)
- immersive simulation and gaming (Jimmy Ivory)
Cross Cutting Approaches
- Systems Thinking (Jake Grohs)
- Human Centered Design (Monifa Vaughn-cooke)
- AI enabled analysis and insight (Michael Hsaio)
Core tool
- Naturalistic clinical interaction data (Sarah Parker)
Our Team
Placing Humans at the Center
Within the complex ecosystem of healthcare delivery, clinicians, caregivers, and patients remain at the heart of real transformation. Technology alone will not fix systemic inefficiencies. Through the Smart Healthcare Hub at Virginia Tech, we are taking a different approach. We see technology as a teammate in a crossdisciplinary strategy to solving the toughest challenges in healthcare delivery.
Our collaboration includes not only clinicians and medical researchers, but social and behavioral scientists, ethnographers, data scientists, tech experts, engineers, and creatives.
By working at the nexus of technology and human behavior — using algorithms and social science to identify new ways to understand the human dimensions of healthcare — we are combining quantitative insights with qualitative understanding to craft human-centered healthcare systems that are more data driven, efficient, and robust.
Through its unique approach to combining both artistic and technical minds to improve conditions for patients and providers — and using technology to achieve better patient communication and readiness — the work of the Smart Healthcare Hub directly aligns with Virginia Tech’s land-grant mission to serve our community.
Furthermore, our rural location enables us to study a population that is not currently well represented in healthcare delivery studies and may be a good proxy for examining healthcare delivery in the U.S. as a whole, as most communities do not have the robust medical resources of major cities.

Patient harm costs the world trillions each year. In high income countries, up to 15% of hospital expenditures can be attributed to wastage due to safety failures. Out of hospital patient harms are difficult to estimate, but they are likely substantially higher. In low-to-middle income countries, as many as 4 in 100 people die from unsafe care, and untold numbers are unintentionally harmed. In the USA, 250,000-400,000 people die each year from unsafe care.
Within the United States in particular, but across the world, healthcare remains expensive and unsafe. This is particularly important for patients in rural locations. Rural patients often live sicker and die younger than their urban counterparts. Technology solutions to improve distance medicine are a crucial part of the solution. Chronic diseases of despair which continue to worsen, which disproportionately impact rural patients. This is a particular need for rural Appalachia and a priority of VT through their history of extremely successful cooperative extension programs.
Patient safety incidents can cause death and disability, and suffering for victims and their families. The financial costs of safety lapses are high for nationalized healthcare systems and can be financially devastating to those without insurance. Reduced public confidence and trust in local health systems has an insidious effect reaching far beyond an individual’s experiences. Health workers involved in serious incidents can also suffer lasting psychological harm.